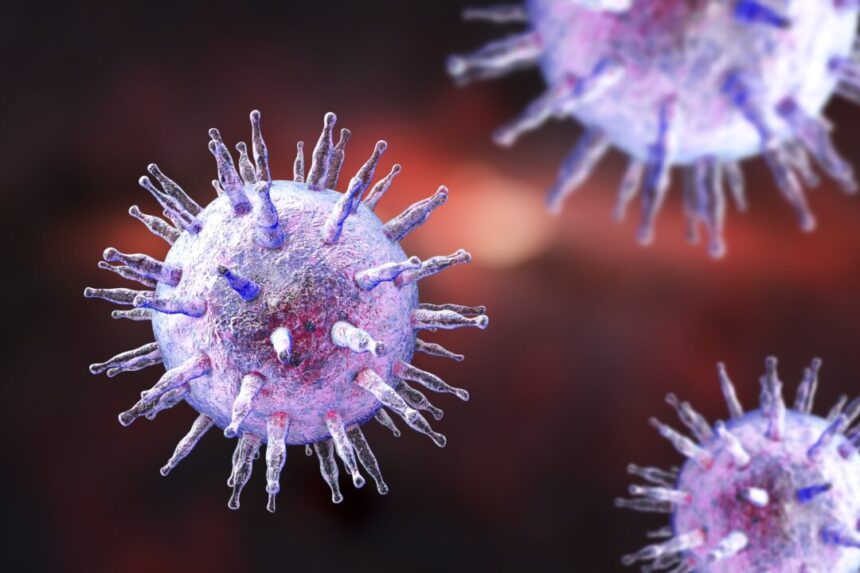
The study’s results have broad implications, as viruses are a significant contributor to global cancer rates, accounting for 10 to 20 percent of cases worldwide. This discovery sheds light on how viruses can lead to cancer, particularly through the mechanism of the Kaposi sarcoma-associated herpesvirus (KSHV).
Researchers at the Cleveland Clinic identified a specific pathway activated by the KSHV virus that influences cell metabolism, growth, and multiplication. By using FDA-approved breast cancer drugs, they were able to inhibit virus replication, halt lymphoma progression, and reduce tumor size in preclinical models.
Lead author Jun Zhao emphasized the importance of understanding how viruses transform healthy cells into cancer cells, as this knowledge can lead to the development and repurposing of existing drugs for more effective treatment of virus-induced malignancies.
Kaposi sarcoma-associated herpesvirus, also known as human herpesvirus 8 (HHV8), is linked to Kaposi sarcoma and certain types of lymphoma. The virus can remain dormant in the body but may become active in immunocompromised individuals, leading to aggressive cancers.
The study found that KSHV virus manipulates host proteins to enhance replication and uncontrolled cell growth, contributing to fast-acting and challenging-to-treat cancers. The prevalence of KSHV is substantial, especially in high-risk populations, although many cases go undiagnosed due to asymptomatic presentation.
In addition to KSHV, several other viruses are known to cause cancer in humans, such as human papillomaviruses, Epstein-Barr virus, and hepatitis B and C viruses. Understanding how these viruses interact with host cells and evade the immune system is crucial for developing effective treatments.
The research team’s discovery of drug combinations that target the hijacked host proteins by the KSHV virus shows promise in reducing tumor size and improving cancer survival rates. This approach could pave the way for new treatment options for KSHV-associated cancers and potentially other virus-induced cancers with similar mechanisms.
Overall, these findings have the potential to revolutionize the treatment of virus-induced cancers by targeting the metabolic pathways hijacked by viruses and cancers for pathogenesis. The future implications of this work are promising, as it may uncover new strategies to combat cancer-causing viruses and non-viral cancers.
Source link