Commentary
Local health care systems across the country are facing a critical threat to their functionality as we know it. The issue at hand is the dwindling supply of effective antibiotics for doctors and nurses to treat their patients, posing a significant risk to the health and financial stability of every American.
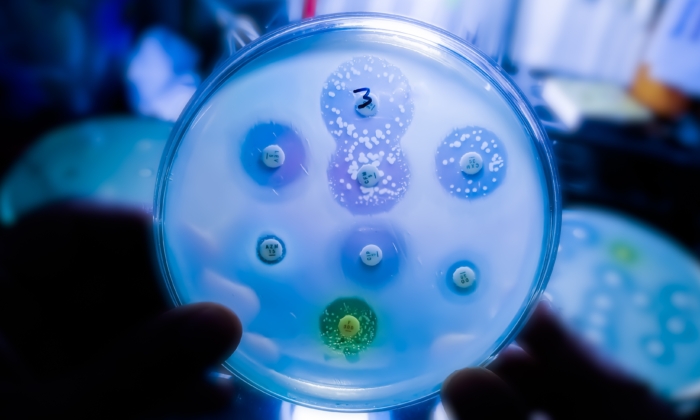
Antimicrobial resistance (AMR) occurs when bacteria and fungi develop the ability to resist the drugs meant to eradicate them. Coupled with a decline in the development of new antimicrobial drugs, AMR poses a serious threat to public health.
If safe and effective antibiotics become scarce, the landscape of innovative medical treatments will need to be reevaluated, potentially undoing decades of progress in medical technology that has improved patient outcomes. The disruption to the health system that would result from the absence of this infection prevention system would have far-reaching consequences.
AMR is not just a health concern but also a financial and national security threat. Drug-resistant infections often require more intensive care and longer hospital stays, leading to increased costs for major federal health programs and patients.
Each year, antibiotic-resistant infections are estimated to cost the U.S. economy $20 billion in direct health care expenses and an additional $35 billion in lost productivity. These costs ultimately burden patients, as resistant infections can add nearly $1,400 to their overall health care expenses.
The ramifications of a world without effective antibiotics are profound. Cancer treatments like chemotherapy may become riskier without the protection antibiotics offer against infections. Many surgical procedures could become too hazardous to perform. The costs associated with redefining medical standards in light of this crisis are immeasurable.
The global impact of AMR is exacerbated by events like Russia’s conflict with Ukraine, which is contributing to a rise in drug-resistant infections in European countries. These infections will eventually reach the U.S., where AMR already claims more lives annually than HIV. The time to act is now.
To combat the overuse of antibiotics and the limited economic incentives for developing new antimicrobials, medical professionals are cautious in prescribing antibiotics. Furthermore, the lack of new antibiotic classes since the 1980s and the financial struggles faced by antibiotic developers pose significant challenges.
The PASTEUR Act, introduced to address these challenges, aims to create a payment model that incentivizes the development of new antibiotics without being tied to sales volume. This legislation could revitalize the development of critical antibiotics and help save billions in costs associated with AMR.
The importance of addressing AMR transcends political divides, and bipartisan collaboration is crucial to finding solutions. By supporting initiatives like the PASTEUR Act, we can pave the way for a healthier future for all Americans.
As a medical professional and a member of Congress, I am committed to prioritizing the passage of the PASTEUR Act to safeguard our health care system. This legislation represents a vital investment in the future of American health and economy.
Recent discussions with experts and policymakers have shed light on the urgency of addressing AMR and the potential solutions at hand. It is imperative that we work together to tackle this pressing issue and secure a brighter future for our nation.
Views expressed in this article are opinions of the author and do not necessarily reflect the views of The Epoch Times.
Please rewrite this sentence.
Source link